 This month I want to address how to treat irritable bowel syndrome. I know it’s not the sexiest topic, but it’s fairly common so I want to offer some education. There are 3 steps: 1. A healthy eating and lifestyle change 2. Symptom-specific diet change 3. Elimination diet. People with irritable bowel syndrome (IBS) have hypersensitive guts that react to certain foods or medications, or to stress and anxiety. It can be debilitating. IBS often comes with bloating, pain, and diarrhea or constipation or a mix of both. Doctors don’t know what causes IBS, which affects an estimated 10 to 15 percent of U.S. adults. They even have trouble diagnosing it. There’s no specific test, imaging, blood marker, or endoscopy that doctors use. It’s diagnosed based on symptoms. Pretty ambiguous huh? And doctors don’t have a great way to treat IBS either. The focus has been on medications that reduce gut spasm, antidepressants that decrease gut sensitivity, laxatives for people with constipation, or anti-diarrheals if that’s an issue. Medications can be very helpful, but try to make some lifestyle changes to help yourself out too, k? So let’s talk about some irritable bowel syndrome remedies and prevention.
This month I want to address how to treat irritable bowel syndrome. I know it’s not the sexiest topic, but it’s fairly common so I want to offer some education. There are 3 steps: 1. A healthy eating and lifestyle change 2. Symptom-specific diet change 3. Elimination diet. People with irritable bowel syndrome (IBS) have hypersensitive guts that react to certain foods or medications, or to stress and anxiety. It can be debilitating. IBS often comes with bloating, pain, and diarrhea or constipation or a mix of both. Doctors don’t know what causes IBS, which affects an estimated 10 to 15 percent of U.S. adults. They even have trouble diagnosing it. There’s no specific test, imaging, blood marker, or endoscopy that doctors use. It’s diagnosed based on symptoms. Pretty ambiguous huh? And doctors don’t have a great way to treat IBS either. The focus has been on medications that reduce gut spasm, antidepressants that decrease gut sensitivity, laxatives for people with constipation, or anti-diarrheals if that’s an issue. Medications can be very helpful, but try to make some lifestyle changes to help yourself out too, k? So let’s talk about some irritable bowel syndrome remedies and prevention.
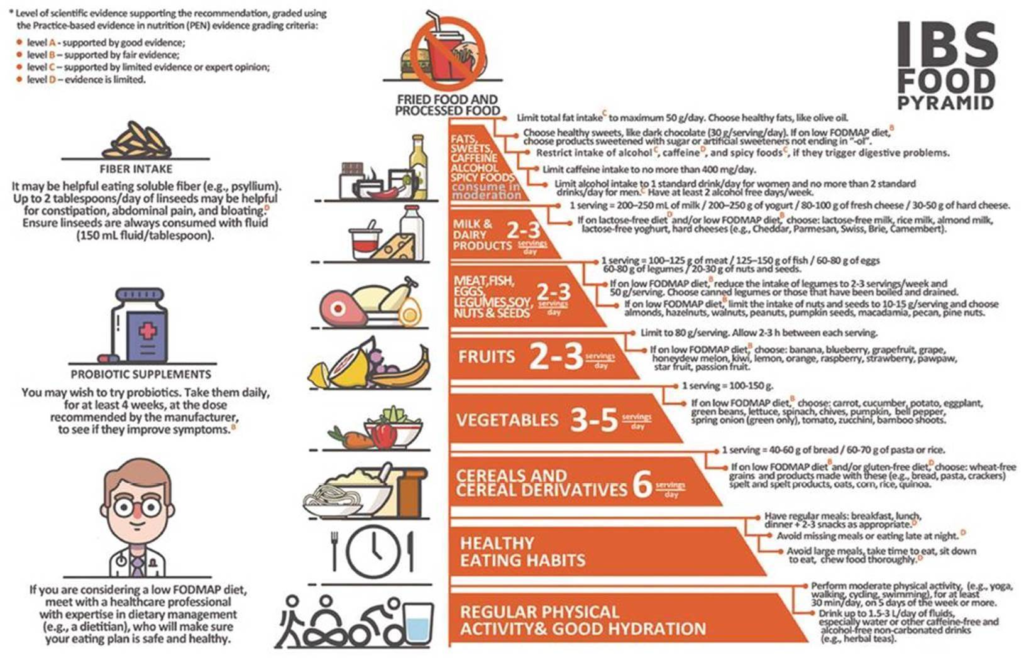
Step One – Healthy Eating and Lifestyle Changes

This includes:
- Plenty of fruit and vegetables
- Choose starchy carbohydrates. Examples include bread, rice, cereals, pasta, potatoes, and bananas
- Some quality (more plant based) protein foods: grass fed meat, sustainable fish, organic or pasture raised eggs, low processed tofu and beans
- Limited amounts of foods high in fats and sugars. Limit saturated fat that is found in animal products such as butter, ghee, cheese, meat, cakes, biscuits, and pastries. Replace these with unsaturated fats found in vegetable oils such as sunflower, rapeseed, and olive oil, avocados, nuts and seeds. Drink plenty of fluid – at least two liters daily, such as water or herbal teas.
- Take time when eating meals
- Have a regular meal pattern and don’t skip meals and eat every 3 hours (smaller meals/snacks)
- Sit down to eat; chew food well
- Try to avoid eating too late at night (2 hours before bed)
- Exercise regularly, such as walking, cycling, or swimming. If finding time is difficult, find time for agonizing symptoms – you feel me?
Manage stress

If you have a chaotic lifestyle, stress and anxiety may also be causing IBS symptoms. I have seen this multiple times with my patients. There are many complex connections between the brain and the gut. Psychological factors, the nervous system, and muscle contractions in the gut all interact with each other, causing IBS symptoms. This is known as the brain-gut axis. So crazy right?! Therefore, stress management can be mega effective in easing symptoms.
- Create time for relaxation for you so you can drop down into that parasympathetic state (I make sure I have 5 min/day to meditate or just breathe; it doesn’t take much)
- Get yourself in nature! Use your senses while you are in it (actually see, hear, smell, and touch)
- Try relaxation therapies such as mindfulness meditation (like insight timer app)
- Exercise!!! If you know me, you know I’m one to tout the medicinal qualities of exercise
- Get enough sleep (7-8 hrs)
- Seek counseling (you take your car in when it’s “not feeling well” right?)
Step Two – Symptom-Specific Changes to the Diet

Sometimes, a healthy balanced diet and lifestyle changes aren’t enough to improve symptoms. It may be that more specific changes to the diet are needed. Many people report that what they eat affects their symptoms. Therefore, modifying what you eat can help to manage symptoms.
Reduce caffeine
Caffeine can stimulate activity in the colon, which may worsen symptoms of pain and diarrhoea. Limit tea and coffee to no more than three cups per day. Filter coffee contains higher amounts of caffeine (140 mg) compared to instant coffee (100 mg) and tea (75 mg). So, if filter coffee is included in your diet, you may want to limit this to two cups per day. There is also caffeine in cola and some other soft drinks, and in chocolate.
Limit alcohol and fizzy drinks
Fizzy drinks and alcohol can worsen symptoms of diarrhoea. Limit your intake of these drinks to improve symptoms. Aim to have at least two alcohol-free days each week and no more than two units each day.
A unit of alcohol is:
- One 1.5 oz shot of spirits
- 1 can of beer
- 5 oz of wine
Reduce intake of resistant starches
These are starches that are resistant to digestion in the gut (small intestine). Therefore, they reach the colon intact and are fermented by the germs (bacteria) in our gut. This produces gases and waste products, leading to symptoms of bloating, wind, and diarrhea. People who have IBS react to smaller doses of resistant starches than those who don’t have IBS. Reducing resistant starches may also improve symptoms of diarrhea.
Reduce intake of foods containing resistant starches
- Highly processed foods such as chips, pizza, and pastries
- Foods that have been cooked and left out to cool – for example, cold potato/pasta salads
- Partially baked bread – for example, garlic bread or pizza bases
- Whole grains, sweetcorn, green banana, and muesli that contain bran
- Dried pasta (use fresh instead)
Cook fresh food whenever possible and eat food that you’ve cooked straightaway. This will help to reduce intake of resistant starches.

Modify your fiber intake
Fiber can be a confusing subject for many of those affected by IBS. For some people, reducing high-fiber foods can help to improve symptoms. For others, increasing fiber can help to improve symptoms, so it is very much dependent on the individual. Adjust fiber intake according to your personal symptoms. Use a food and symptom diary and monitor any changes. Try to dose slowly with fiber so that your overall health can improve.
It may help to clarify what exactly dietary fiber is and how it may affect symptoms. There are two types of fiber which work differently in the body. Generally, reducing insoluble fiber may help with symptoms, but if an increase in fiber is necessary, this should be from soluble fiber.
Insoluble fiber
This type of fiber does not dissolve in water and is not readily broken down, so it passes through the digestive system mostly intact. It absorbs water, adds bulk to stools, and allows waste to be passed through bowels more quickly. Reducing this type of fiber may help to improve symptoms of diarrhea. Foods to reduce or avoid:
- Skin and pits of fruit and vegetables (if it bothers you)
- Wheat and bran
- Corn (maize)
- Nuts and whole grains (if they bother you)
Soluble fiber
This type of fiber dissolves in water and is broken down by the natural bacteria in the bowels. It softens stools and makes them larger. Increasing this type of fiber may help to improve symptoms of constipation. Foods to include are:
- Oats
- Barley
- Psyllium
- Nuts and seeds
- Fruit and vegetables
- Beans and pulses
Whole grains (for example: wholemeal bread, brown rice, and wholewheat pasta) may also help with constipation. Although increasing fiber may help to improve symptoms, it may also generate gas and cause pain and bloating. Monitoring is important to help identify this and to adjust your fiber intake according to your symptoms.
If fiber intake is suddenly increased, this can cause symptoms of wind and bloating. Introduce high-fiber foods gradually to allow the gut to become used to the extra fiber. Introduce one new food over a two to three-day period and monitor any symptoms. For example, have oats for breakfast on the first day, then add beans or extra vegetables to a casserole two days later, then maybe have an extra piece of fruit two to three days later.
Drink LOTS of water
Fiber needs water, so aim to drink at least 8-10 cups of water daily or other fluids such as herbal teas. People with diarrhea will need to make sure they are replacing these lost fluids. Drinking water will also help to improve constipation.
Include golden linseeds
Including these in the diet may improve symptoms of gas, bloating, constipation, and diarrhea. They are a source of insoluble and soluble fiber. They can be added to casseroles, stews, soup cereals, yogurts, and desserts. Include one tablespoon each day.
Reduce fatty foods
Some people find that fatty foods are difficult to digest and can cause symptoms of diarrhea; therefore, reducing fat in the diet may help:
- Limit cakes, biscuits, chocolates, and pastries
- Cut down on fatty meat products such as sausage
· Use lower-fat dairy products – for example, low-fat yogurt, cottage cheese, low fat milk. - Choose tomato-based sauces rather than creamy sauces – although some tomato sauces can be oily, so check the label!
- Use small amounts of cheese (a matchbox size is a portion) – stronger-flavor cheeses may help you to use less… just a thought
- Take care when using dressings and sauces such as mayonnaise and salad cream. Use small amounts and try the reduced-fat versions
- Cut off visible fat from meat and choose leaner cuts of meat; use pasture raised if possible
- Use minimal oil/butter when cooking (use an oil spray, or measure using one teaspoon of oil per person, per meal)
- Try different cooking methods such as steaming, boiling, microwaving, grilling, and poaching rather than frying
Reduce fructose
Fructose can cause diarrhea in some people, particularly when eaten in large quantities. Sometimes fructose is not well absorbed; it can draw water from the body into the bowel, causing osmotic diarrhea. If fructose is not well absorbed, it is fermented in the colon and gases are produced, causing gas and bloating in some people with IBS.
Try limiting fruit intake to no more than three portions each day. Only have one small glass (4 oz) of fruit juice per day. Having more vegetables will help to meet the recommendation of at least five portions of fruit and vegetables each day. A portion is about what might fit in the palm of your hand. A portion of dried fruit is about one tablespoon.
It might be useful to limit honey, which contains fructose. Sometimes ‘high-fructose corn syrup’ or ‘corn syrup solids’ are added to processed foods, so try avoiding or limiting these. Check the labels for these ingredients.
Avoid sorbitol
Sorbitol is poorly absorbed and has a laxative effect when it enters the colon, so this can cause symptoms of bloating and diarrhea. People with IBS may be sensitive to smaller amounts of sorbitol.
Sorbitol is found in artificial sweetener, low-sugar sweets, drinks, mints, and gum, and often found in diabetic products. Also check the labels of these products for mannitol and xylitol, which have a similar effect.
Take probiotics! Like now!
Probiotics may be useful in improving symptoms of IBS, although they do not work for everybody. Probiotics can help to balance our gut bacteria. The ‘good’ bacteria in probiotics compete with ‘bad’ bacteria for space in the gut. This means that there are fewer ‘bad’ bacteria, making it a healthier gut environment. This can help with digestion and to improve symptoms of gas, bloating, and diarrhea (not to mention immune and mental health).
There are a number of probiotic products available, including yogurts, drinks, and supplements such as tablets and capsules. My latest faves are Pro45, Align, and Florastor. Probiotics need to be taken in the recommended dose every day for at least four weeks. DAILY, k? Monitoring symptoms can help to identify any benefit. Other brands contain different mixtures of bacteria, so trying a different product may help if there is no success with one particular brand. I suggest switching up brands when you run out of the bottle anyway. I take one every single day.
Step Three – Elimination Diets

Some people find that even after making these dietary changes, their symptoms are still not improving. Avoidance of single foods or following elimination diets might have some benefit for people with IBS. Such dietary regimes should only be followed with the guidance of a Registered Dietitian and/or Gastroenterologist.
Food intolerance
Some people with IBS may have a food intolerance. Some food intolerances, such as lactose, can be diagnosed with a hydrogen breath test, which can be arranged by a doctor. Other food intolerances can be identified by following a diet that excludes suspected foods.
If it is thought that particular foods are causing symptoms, a dietitian (like myself) may advise you to exclude these foods for a certain time period. This is to monitor whether symptoms improve when these foods are taken out of the diet. After this time period (usually 2-4 weeks), the foods are gradually re-introduced to see if symptoms come back. Common intolerances include lactose (found in milk and dairy products), wheat (found in bread, cereals, and pasta), and caffeine (found in tea, coffee, or cola).
The low FODMAP diet
There is a growing body of evidence that the low FODMAP diet is effective in improving symptoms of IBS. FODMAP stands for:
- Fermentable
- Oligo
- Di
- Monosaccharides
- And
- Polyols
These are a group of short-chain carbohydrates that are not very well absorbed in the gut (small intestine). These carbohydrates are easily fermented and cause more fluid to enter the large bowel, leading to gas, bloating, and diarrhoea. Reducing the total amount of these fermentable sugars may improve IBS symptoms. The low FODMAP diet should be tried with the assistance of a Registered Dietitian and/or Gastroenterologist. I know I’m repeating myself. 😉
If you need more support with this, don’t hesitate to reach out. Remember you really do have power over your body.
Health can be yours!
Miriam
MPH, R.D., CPT, Certified Intuitive Eating Counselor
Resources:
2. http://myginutrition.com/diet.html
3. U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th Edition. https://health.gov/dietaryguidelines/2015/guidelines/. Published December 2015. Accessed March 2, 2017.








Comments - 0